Pathologizing Normal: Distress is not Mental Illness
Concept creep and influencers on commission suggest otherwise, but you don't need therapy for everything
This is Part 5 of a five-part series on why distress is not damaging.
Today’s post rounds out the series with a longread, so make yourself a cuppa, put your feet up, and settle in…
In bed, a pyjama-clad off-duty therapist sits, enthralled by a podcast on Youtube, only to be rudely interrupted by an ad for BetterHelp.com. It’s an Inception embed, clearly cut from another Youtube video. A young influencer, probably not a day over 20, sits in her car with takeaway food on her lap, and enthusiastically offers up her “number 1 tip to get over a breakup.” Going to therapy.
She says she’s been going two to three times a week, and that brings her to the sponsor of today’s video: BetterHelp.com, the world’s largest therapy service, 100% online. “You can actually message your therapist at any time,” she says, like that’s a good thing for healthy boundaries. And therapy is, according to this non-mental health professional, for anyone, at any time, for pretty much any thing.
Tyres screech as I hit the brakes. Back this old rustbucket up for a closer look.
There’s a few claims here to unpack. But first, let’s address the fact that this was an ad delivered by a walking billboard without a prefrontal cortex, not a recommendation from a mental health professional. And the walking billboard is either receiving sponsorship dollars for hosting the ad, or a flat-rate commission on every customer conversion via affiliated links.¹ Turns out mental health marketing is big bucks for influencers. I’ll let you question the ethics of that.
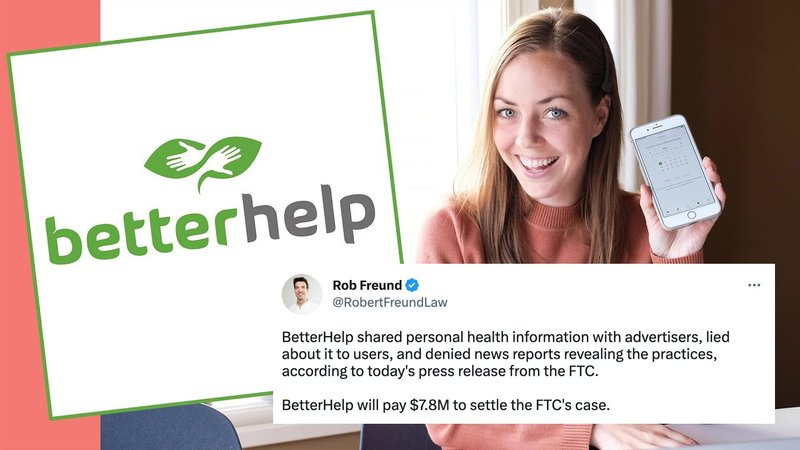
Better Help?
BetterHelp.com operates on a subscriber model, kind of like Spotify, except instead of all the choons you want for whatever mood you’re in, it’s 24/7 access to a therapist, for whatever mood you’re in.
More subscribers means more revenue. That means company shareholders have skin in the game when it comes to convincing you that you need therapy. So do the influencers who do their marketing for them. Concept creep bleeds through social media.
Proponents claim the online-only model is cheaper than other models of therapy, but at $90-$120 Aussie dollars per week, it’s basically the same as the cost of seeing an unsubsidised counsellor, or the gap fee you pay when you see a Medicare-subsidised psychologist, both of which can also offer you online or phone appointments. And while a lot of insurance providers cover therapy that originates on terra firma, they do not cover BetterHelp. Thankfully, for folks without even modest means to pay for therapy, there are free-of-charge services on terra firma run by non-profits. Those tend to be staffed by big-hearted professionals with a passion for public service and specific expertise at the pointy end of mental health.
Realistically, BetterHelp may work out a fair bit pricier than standard therapy. You can get up to four sessions per month, and these range from 30-45 minutes, as opposed to the 50 minutes you get as standard in the terra firma therapy model. But there’s no middleman pocketing a chunk of that for shareholders, so I guess standard practitioners don’t need to charge as much. And they only charge you for each session, however often you need them; they’re not asking you to pay in advance for a month’s worth of sessions you might not actually need or be able to schedule in. The subscriber model may be encouraging a higher-than-average level of usage to get you bang for your buck.
There’s real limitations to what you can achieve in a 30-minute timeslot if you’re getting actual therapy – you know, where you learn and practice skills, not just debrief on your week. If you think the opportunity to text your therapist 24/7 makes up for that, then consider the fact that BetterHelp has no guidelines for how quickly your therapist must respond to you. Anecdotally, there’s a wide diversity in response timeliness, frequency, and quality, with a lot of responses being vague and generic, or just asking the client to wait until the next live session.
I’m not convinced we should be expecting our therapists to be responding all hours of the clock, though. Therapists are too well-versed in self-care and boundaries to sign up for a sweatshop model of work. And one would hope they’d model said self-care and boundaries for their clients too. So I have nothing against therapists asking clients to hold on until the next session; I have something against the platform promising a higher level of contact at a premium when they can’t guarantee follow-through.
Why the $90-$120 range, though? Do you get more if you pay more? Nope. The range is because they operate according to a ‘surge’ pricing model, like that used by rideshare company Uber, whereby prices are bumped up where demand is higher.² So bad luck if you live in a busy metropolitan area but aren’t a high earner. Imagine having to pay more for cancer treatment just because a lot of other people also need cancer treatment. Again, I’ll let you mull the ethics of that.
Also note that in the online-only model therapists can’t provide diagnoses. That’s not a problem if you don’t care for diagnosis, but if a diagnosis would help you, then you’re not getting that help at BetterHelp. Most licencing boards worldwide require diagnoses to be made in person by a therapist who can observe the client over the course of multiple sessions, making note of their physical presentation well as the things they say. Anecdotally, I have heard about users receiving speculative diagnoses from their BetterHelp providers. I can’t verify that, but if it’s happening, please note that it should not be, and is in breach of professional ethics. Online-only therapists can evaluate your symptoms and suggest what they may indicate, and then suggest possible therapeutic interventions that may match the symptom profile. But without the opportunity to see you in person, they cannot complete a full workup, so their diagnosis would be at higher risk of inaccuracy; hence they are prohibited from providing one if they haven’t met you in person.
What about the increased privacy and anonymity promised by online services, though? Well BetterHelp did just happen to settle with the FTC last year for $7.8 million (USD) over their provision of confidential subscriber metadata to third parties for targeted advertising purposes.³ That means service users are the product as well as the consumer. I think we call that exploitation. The privacy breach is, of course, something you could sue your therapist for if they did it, something that could get them deregistered. Goodness only knows what they’re paying their therapists if they happened to have $7.8 million in spare change available for a federal lawsuit and still crank a profit. It’s quite possible a bunch of people with letters after their names spent tens of thousands on qualifications that are getting them paid the same as a teenage burger flipper. Though the end user has no way of actually confirming the credentials of the therapist they’re working with, what with the lack of transparency around how the platform itself vets service providers.¹ If you go to see a therapist on terra firma, on the other hand, their verified credentials have to be on display.
But back to the main point of this post. The influencers’ lucrative project is to convince you, through concept creep, that you need therapy. So, do you?
Let’s unpack the claims in the ad.
1. Is therapy useful for things other than mental health issues?
Yes and no.
I’ll start with the yes. You don’t need a major mental health crisis to benefit from seeing a mental health professional. A Medicare-subsidised clinical psychologist really should only be taking clinical cases, as they’re paid a premium to do specialised work. But counselling (which isn’t Medicare-subsidised, but which is covered by a lot of health insurers) is genuinely supportive for tackling a range of life stressors including life transitions, grief and loss, relationship concerns, major decisions that require a sounding board, for upskilling in areas such as self-esteem, social and communication skills, and for challenging self-doubting or perfectionistic tendencies. So long as there’s a clear-cut problem for which the therapist is qualified to help you find a solution, then counselling is a suitable option.
But what about the walking billboard’s advice about seeing a therapist to get over a breakup? Well, that classifies as a potentially stressful life transition, so I’m not ruling out the possibility that it could be helpful. But perhaps check in with your social support network as first port of call. Most people have at least one understanding shoulder they could cry on. I mean, do you know anyone who hasn’t been through a breakup? Do you seriously not know anyone who could empathise with what you’re going through? Most of us have a social network that offers us a buffet of options suitable for such times: a shoulder to cry on, frivolous fun to distract us, some wise words based on experience, a couch to crash on, or a helping hand to move house. Therapy might be useful if, after a few weeks have passed, you still find yourself struggling to show up for life, unable to concentrate on things, preoccupied with your loss, ruminating over things that were said or done. Go to therapy if that’s where you’ve landed after a few weeks have passed. But otherwise, no, a breakup is not a condition that impacts wellbeing and functioning, and you don’t need therapy for it.
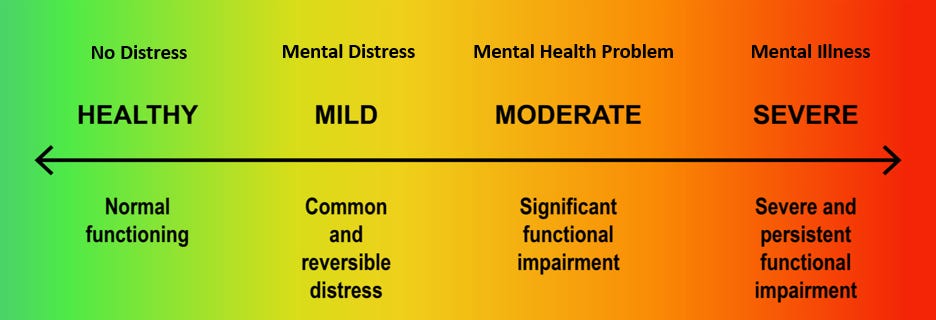
The line in the sand must be drawn somewhere, and the high-tide mark seems to make sense. The current social media-fuelled zeitgeist has it that young people in particular are self-pathologizing every little thing that feels uncomfortable. Just like how a hypochondriac focuses on every little twinge, someone who’s self-pathologizing may see every flicker of nerves as anxiety, or every down day as depression, or every challenging event as trauma. Concept creep even has some of us believing that the things people say to us could cause trauma. They cannot. The word ‘trauma’ has seemingly been repurposed to mean discomfort. We therapists need to reinstate its true meaning lest we be overrun by a tsunami of garden variety teenage angst while actual trauma clients languish on waiting lists.
Discomfort is just a fact of life, and distress comes with the territory. Just because toxic positivity doesn’t work for us doesn’t mean we’re somehow broken. Toxic positivity simply doesn’t work; it’s not fit for purpose. Life is challenging, things come up that make us angsty or get us down, and we face obstacles that need to be overcome. I cannot say this clearly enough: This. Is. Life. We will have shit days, and we will be ok. If there’s one thing someone who’s self-pathologizing could benefit from seeing a therapist for, it’s this: boosting distress tolerance.
2. How much therapy should you be getting?
The idea that more isn’t necessarily better isn’t new. Most therapists suggest clients attend appointments on a weekly or fortnightly basis, and this tapers off as therapeutic goals are reached. You might think you could make more progress if you were to attend more frequently, but that assumes you can cram ‘the work’. We’ve all tried cramming for exams and assignments at some point, right? Now, tell me: how much of what you crammed do you remember now?
In reality, ‘the work’ takes time. Your therapist will assign you ‘homework’ between sessions because that’s where the real work gets done. In session, you excavate, you gain insights, and you learn skills. Outside, you percolate, you assimilate, and you practice your newly learnt skills. It’s easy to see why most therapeutic advances happen outside the consulting room. And that doesn’t for a minute negate the value of time spent in the consulting room. It’s just a point of perspective: spending more than a session a week in consults isn’t likely to speed up your progress. Excavating isn’t generally rapid; it’s more like how archaeologists work, delicately chiselling and brushing away fragments of dust that obscure the full picture. And insights don’t tend to come all that thick and fast; the brain takes time to assimilate them. And skills can’t be rushed if they’re to be honed.
So, what’s the value of 24/7 contact with your therapist? Well, aside from the perception that this is providing you with a flexible and responsive model of care, the value is limited. In reality, other models also provide flexible and responsive care. Since COVID forced us all online in 2020, most therapists I know offer a hybrid model whereby you can attend sessions in person, online, or via phone, and most therapists respond to emails and phonecalls between sessions, albeit during their stipulated business hours. Because they have lives, families, self-care needs. It’s also true that most clients don’t actually need to email or phone their therapist between sessions. The option is there, but generally folks can hang on until the next session. A few adulting skills come into play here: patience, distress tolerance, and healthy boundaries.
Influencers on commission are telling us to expect therapy on demand like it’s pay TV. But you don’t need 24/7 therapy any more than you need to be able to access Game of Thrones re-runs on your commute to work. You stopped needing attention to your every whimper once you exited infancy. You can hold on. You can note down your thoughts in a journal, and bring these up at your next session. And when you’re struggling with big feelings between sessions, put those distress tolerance and emotion regulation skills your therapist taught you into practice. And if they didn’t teach you those, then find a new fucking therapist, cos the last one didn’t do their job.
3. Should you be subscribed to therapy long-term?
No.
I want to end this section here, but an explanation is probably needed. Your therapist, if adequately trained, will come up with a case formulation that is specific to your concerns, and will identify appropriate targets for intervention based on this formulation. For any given intervention target, there is an intervention protocol that is anchored in evidence, and should be workable within a certain timeframe. While I think it’s inhumane that Medicare subsidises so few therapy sessions for any given individual, the reality is that a lot of issues can be addressed in large part in just a handful of sessions.
Take anxiety for example. The key mechanism is avoidance, so that’s a common intervention target. The goal of therapy is to help the client to reduce their avoidance of anxiety-inducing stimuli to the point where they can go about life fully. This doesn’t mean they’ll never feel any anxiety ever again; it means they’ll be fully functional and have a good level of wellbeing in spite of feeling some anxiety sometimes. Why? Because their anxiety won’t be dominating their life; they’ll be able to face things that induce anxiety, and take charge of life. Exposure to anxiety-inducing stimuli can start as soon as the target is identified and the client and therapist agree on the goal. Clients have been known to make enough gains in the space of a single exposure session to be able to get back on with their lives with minimal disruption to functioning and a pretty good standard of wellbeing. Most people only need a handful of sessions to nail it. If you’re in long-term therapy for anxiety, find another therapist. Talking about your anxiety doesn’t make it go away; facing your anxiety is the key to functioning and wellbeing.
The same goes for most things: they can be addressed in a relatively short course of therapy provided you stay focused and do the work. A few weeks to a few months should do it. Of course it can be helpful to retain contact with a therapist after a particular goal has been attained. You might want to check back in down the track to tackle different goals, or you may have occasional check-ins as part of a relapse prevention plan. But a therapist who keeps you in regular sessions long term may be either placating your neediness that they should have addressed as a therapy target, or they may just be predatory.
4. Do you actually need therapy?
After everything I’ve said you might now be thinking there’s little call for therapy unless you have a diagnosed/diagnosable condition. I don’t want to give that impression. There is definitely benefit to therapy for a multitude of reasons beyond mental ill-health. But it’s important to tap your supports and resources as well, as these are going to remain your supports and resources after your course of therapy is finished. And if you start there, you may find your needs are covered and you don’t need therapy at all. Don’t assume therapy should be your first port of call. Sometimes it’s a lifestyle shift you need, and starting there will save you time and money on your therapist checking off on those basics.
Am I trying to do us all out of a job? No. But before I jump to the conclusion that my client’s concerns require psychotherapeutic intervention, I need to know a few things about their lifestyle and circumstances. So, here’s my starting blocks checklist so you can check some things off for yourself before spending your hard-earned money on a mental health professional.
Sleep
First and foremost, I ask about my client’s sleep, in terms of quality as well as quantity. Do they have a regular sleep routine where they get up and go to bed at around the same times every day? Are they sleeping through the night and waking up refreshed? What might be getting in the way of a healthy and consistent sleep routine for them? Getting sleep right shunts a lot of other Tetris blocks into place, making us more resilient to stress. So it makes sense as a starting point for functioning and wellbeing.
Exercise
Then I ask about exercise. Firstly, is my client exercising at all? We all need to be exercising within the bounds of our capability, and most people really aren’t doing enough. If you’re managing to rustle up an endorphin or two a few times a week, then eating right and sleeping well get easier, stress becomes more manageable, and baseline mood elevates a notch or two. I cannot extol the virtues of exercise enough. In fact, I’d go as far as to say I literally ran my way out of a prolonged and arduous depressive episode in my early thirties.
Diet
I lose count of the number of clients I’ve seen who just don’t eat right. Whether it’s packing junk food, skipping meals, emotional eating, or relying on convenience at the expense of nutrition, it’s easy to get it wrong. I understand that a lot of us are time-poor, and not everyone enjoys cooking enough to push open a window of time for it in a busy schedule. But when you get it right, with the right balance of protein and fibre from mostly wholefood sources, you notice a difference. It’s a matter of prioritising, and there’s a range of options for the time-poor among us. It’s also well worth getting your bloods done to see if you’re low or deficient in anything, as iron, magnesium, B12, Omega 3, and D3 deficiencies are relatively common, and all affect both physical and mental health. There’s a veritable rabbithole of nutritional psychiatry I could go down here, but it’s out of my lane, and thus unethical to take you with me. So, check in with an expert if you find yourself deficient and needing to make changes.
Alcohol and other substances
I also have to ask my clients about their relationship with alcohol and other substances. Even for those of us who’ve never considered we might have a substance issue it’s worth checking in on how often we consume substances, and under what circumstances. Are you able to take days off? Weeks? How much do you consume in any one sitting? Regardless whether a substance has a hold over us, most of us benefit from reassessing our relationship to our chosen vices, not least because they affect our sleep quality, nutrient absorption, exercise tolerance, and resistance to stress.
Social supports
Once I’ve got the physical health questions out of the way, we move onto the social sphere. It’s important to understand what my client’s relationships with their family and significant others are like. For some, these are great sources of support and strength, while for others they may be the primary cause of stress. And for others, they may be grieving the loss of valued connections or the connections they never had. Friends and acquaintances also feature here, and for some people they fill in the gaps left by a frayed family network. I like to ask my clients if they have at least one friend they could call at 3am in an emergency, and that includes if they’re having an existential meltdown and need a shoulder. A lot of people do have this person, but they don’t necessarily make use of the resource. This is particularly true for men, many of whom say they don’t have someone they could call a close friend at all, but who do have existing relationships that could be strengthened in this way.
Work and employment
I also ask about work and employment for three key reasons. First, financial security is an issue no mental health intervention is going to address. If my client doesn’t have financial security, then cognitive reappraisal isn’t going to get it for them. A different kind of intervention is needed. Secondly, the work itself may be the main source of stress, so this needs unpacking. And lastly, work provides us with a sense of meaning and purpose if we’re in the right role with the right team, even if the work itself is physically demanding or monotonous. For a lot of people, a change in circumstances might make all the difference.
Leisure and hobbies
It might seem trivial, but I also ask about leisure and hobbies. We all need downtime, and so I ask my clients how much they’re getting and how they’re spending it. Some people are burning themselves out and aren’t getting enough leisure time, so they need to make space to simply recharge. Others aren’t spending their leisure time in a way that’s meaningful or purposeful, and this is a relatively easy fix. The addition of meaning and purpose through creative or expressive pursuits, personal challenges, learning goals, volunteering, or passion projects helps build up our sense of who we are, elevates self-esteem, and provides us with additional strings to our bow that buffer the stress of things not going so well in the realms of work, family, partnerships, or health.
Life events
And, lastly, I have to ask whether anything has happened in my client’s life that might have led to the way they’re feeling. It could be that the loss of a loved one, a major life transition, or a potentially traumatic event has brought them to see me, even if they’re initially unaware of that connection. In trauma therapy, the event, or string of events, is the starting point for establishing whether my client is struggling with a trauma- or stressor-related disorder, or perhaps just working through the aftermath of a potentially traumatic of stressful event and need a little support to help them on track. All of the other resources, be they physical health, social support, or sources of meaning and purpose, are all protective factors I like to ensure my trauma clients have and can build on too, as recovery from trauma is hard work, and we need all the resources we can muster.
The TLDR
What am I getting at here? Well, a lot of the time people don’t actually have mental health issues at all; they just have lives that could use some improving. Maybe it’s a health kick they need, or a career change, or a new set of friends. Maybe they just need a creative outlet. Maybe they need a bit of a reset on a lot of things. Most people can manage that for themselves once they realise what’s missing and what they need to work on. A lot of people still benefit from the support of a therapist to help them work out what needs doing and what steps will get them there. And that’s something I genuinely like working on with clients, as I get to see real gains in short time, and clients go away with a sense of mastery over their lives.
But the bottom line is a message most people should actually find quite empowering: statistically speaking, you probably don’t have a mental health problem, and you probably don’t need therapy to get well. You may need to make some changes that are well within your sphere of influence. And you may benefit from a sounding board or someone to help hold you accountable to yourself. And you may just need to practice saying hard stuff out loud in a supportive setting before you feel brave enough to talk to friends and family about things that are troubling you. I’ve been there too, and it made the world of difference to nut it out with a counsellor first before opening up to people who would still be there for me for years to come once my sessions were up.
Simply put, distress is normal, not pathological. We should expect to experience it. We should not expect to be able to eliminate it from our lives. We should accept that sometimes we just have to feel it, and then get on with life. Sometimes life just sucks for a bit. But we take steps to make it better, and it does get better.
So, I’m not here to validate the notion that we all need therapy for every little emotional twinge we feel. Over-validating is a thing, and it’s a slippery slope to nowhere good. The sick role is a self-fulfilling prophecy, and it takes the best years from too many people’s lives. You can face adversity and you can get through hard times. You’re here to tell the tale, aren’t you? And if you need to see a therapist to kickstart that process, do that.
But don’t go pathologizing yourself or anyone else based on feeling bad. None of us get to feel good all the time. But distress isn’t damaging, and it’s only one of the feelings we get to feel in life’s many-textured tapestry of feels.
References
Deltombe, N. & Bachmann, F. (2021). How the BetterHelp scandal changed our perspective on influencer responsibility. Maastricht University. https://www.maastrichtuniversity.nl/blog/2021/02/how-betterhelp-scandal-changed-our-perspective-influencer-responsibility
Owens, H. & Blanton, R. (March 22nd, 2024). We Had 7 People Try BetterHelp: Here’s Our Review. Verywell Mind. https://www.verywellmind.com/betterhelp-online-therapy-review-4777097
Federal Trade Commission. (March 2nd, 2023). FTC to Ban BetterHelp from Revealing Consumers’ Data, Including Sensitive Mental Health Information, to Facebook and Others for Targeted Advertising. https://www.ftc.gov/news-events/news/press-releases/2023/03/ftc-ban-betterhelp-revealing-consumers-data-including-sensitive-mental-health-information-facebook



Excellent work. Thank you.